Bcbs Reconsideration Form
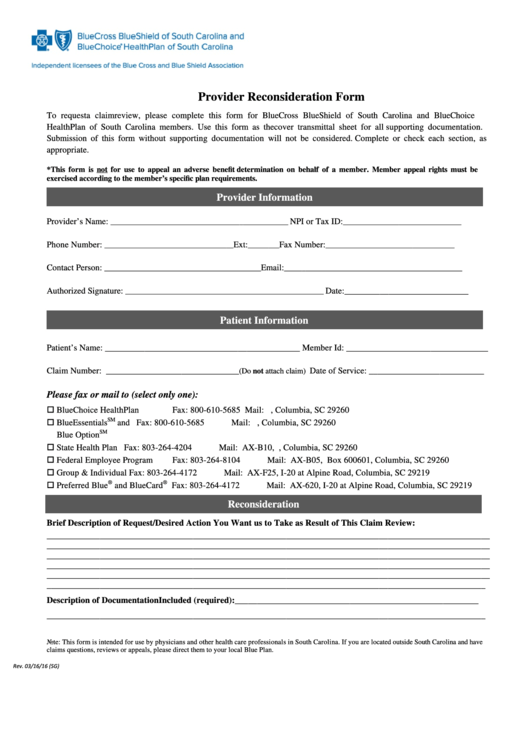
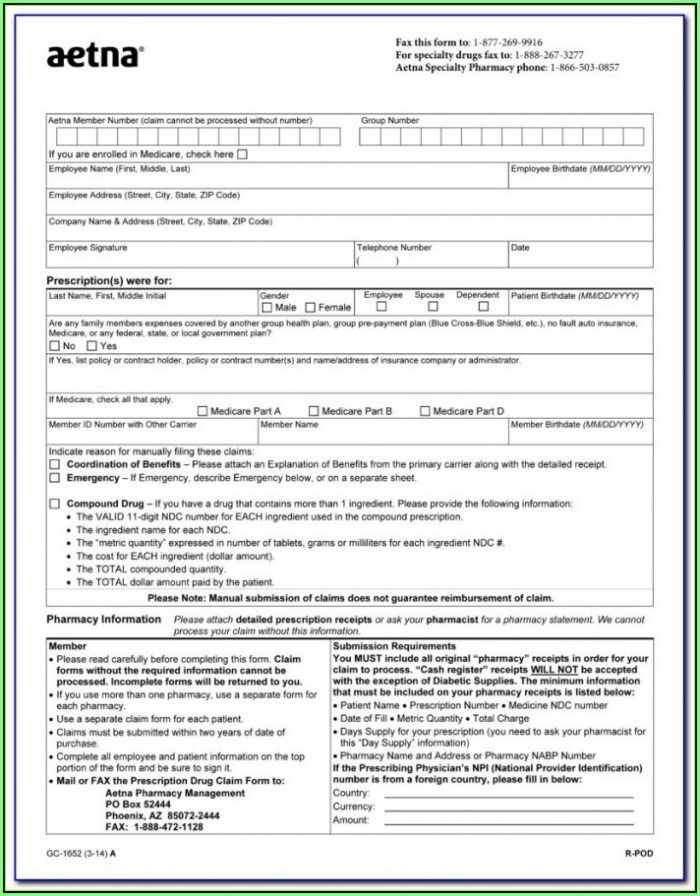
Bcbs Reconsideration Form - Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request. Web this form is only to be used for review of a previously adjudicated claim. Send the form and supporting materials to the appropriate fax number or address noted on the form. Most provider appeal requests are related to a length of stay or treatment setting denial. Here are other important details you need to know about this form: Manufacturers invoice for pricing (attached)copy of subrogation or worker's compensation* This is different from the request for claim review request process outlined above. Original claims should not be attached to a review form. For additional information and requirements regarding provider
Here are other important details you need to know about this form: Skilled nursing facility rehab form ; Operative reports, office notes, pathology reports, hospital progress notes, radiology reports and/or lab reports. Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request. Web when submitting a provider reconsideration or administrative appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for physician and providers available online at floridablue.com. Specialty pharmacy / advanced therapeutics authorizations; Radiation oncology therapy cpt codes; Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Web please submit reconsideration requests in writing. A request to blue cross and blue shield of nebraska (bcbsne) to review a claim with additional information not previously provided.
Web provider reconsideration helpful guide; Web when submitting a provider reconsideration or administrative appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for physician and providers available online at floridablue.com. Specialty pharmacy / advanced therapeutics authorizations; Reason for reconsideration (mark applicable box): Radiation oncology therapy cpt codes; Most provider appeal requests are related to a length of stay or treatment setting denial. Web this form is only to be used for review of a previously adjudicated claim. A request to blue cross and blue shield of nebraska (bcbsne) to review a claim with additional information not previously provided. Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request. Manufacturers invoice for pricing (attached)copy of subrogation or worker's compensation*
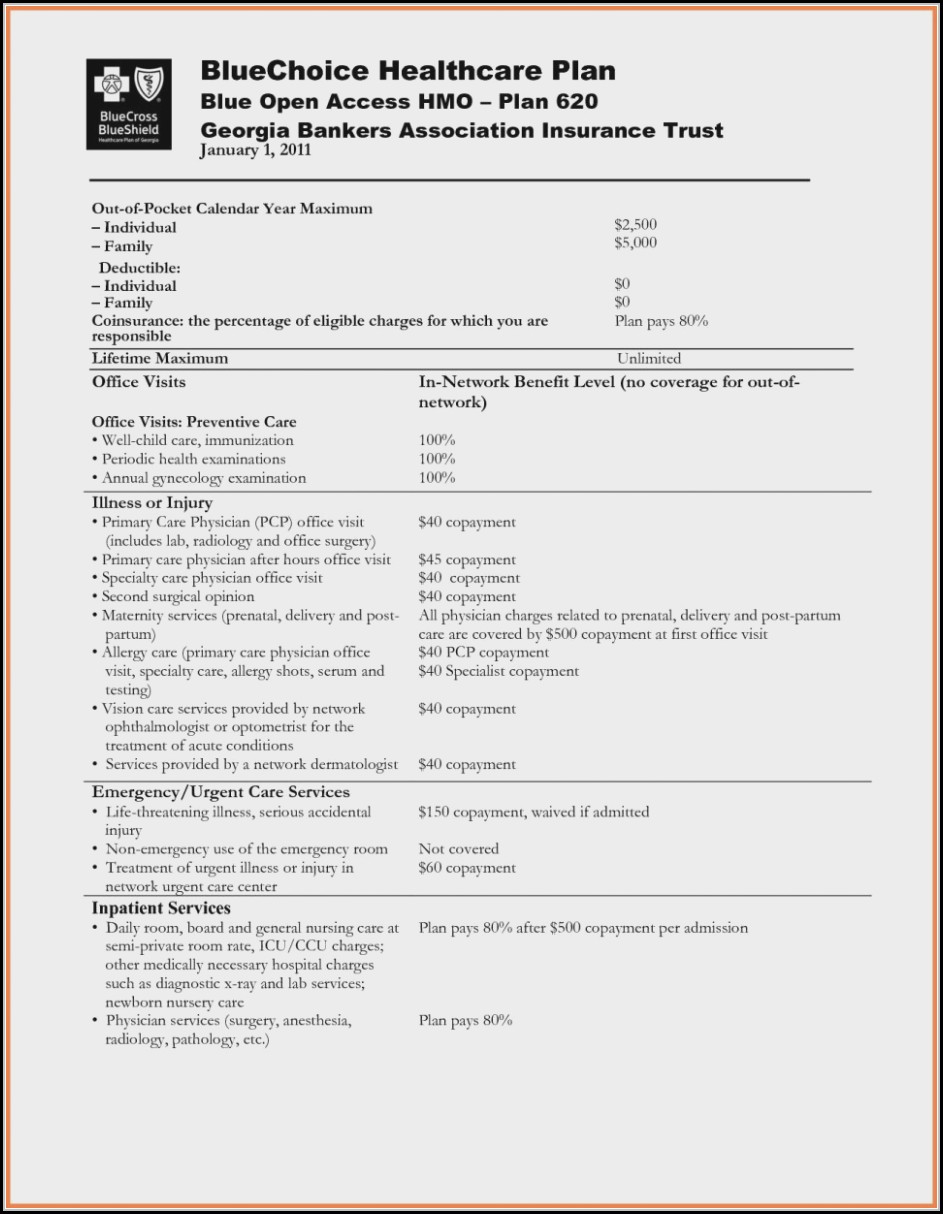
Bcbs Prior Authorization Form Medication Form Resume Examples
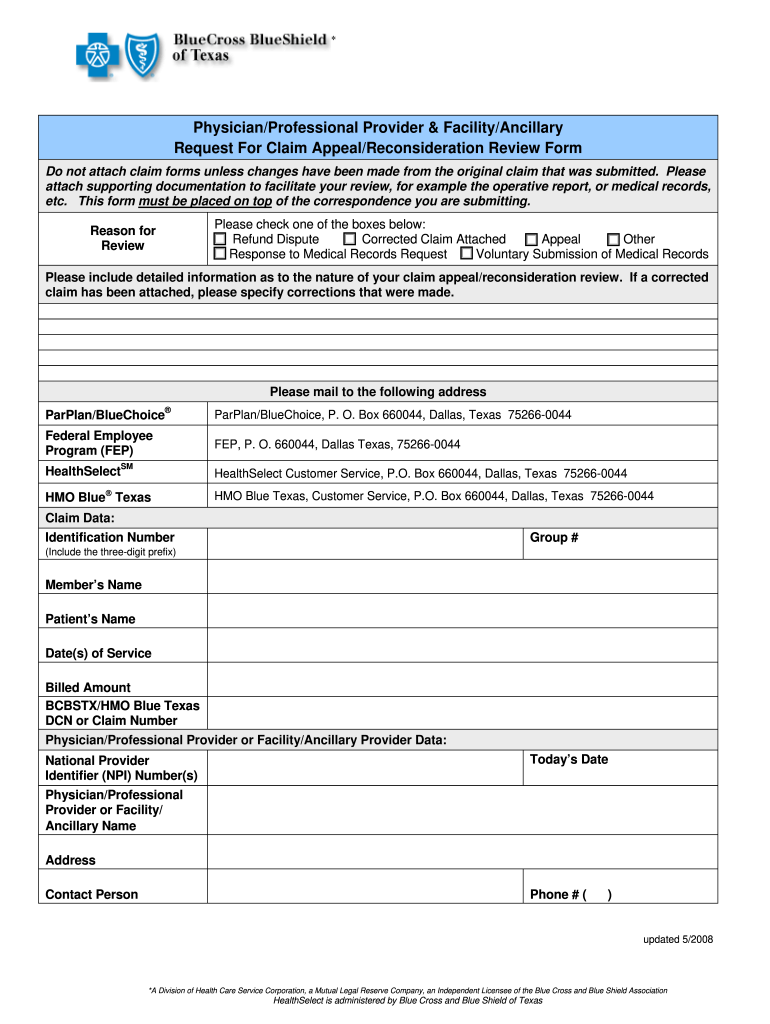
Radiation oncology therapy cpt codes; Access and download these helpful bcbstx health care provider forms. Web this form is for all providers requesting information about claims status or disputing a claim with blue cross and blue shield of illinois (bcbsil) and serving members in the state of illinois. Web provider reconsideration helpful guide; Here are other important details you need.
Blue Cross of Mass giving opioid overdose reversal kits to
This is different from the request for claim review request process outlined above. Skilled nursing facility rehab form ; Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Manufacturers invoice for pricing (attached)copy of subrogation or worker's compensation* Do not use this form to submit a corrected claim.
Highmark BCBS Form ENR010 20142021 Fill and Sign Printable Template
Specialty pharmacy / advanced therapeutics authorizations; Web please submit reconsideration requests in writing. Only one reconsideration is allowed per claim. Send the form and supporting materials to the appropriate fax number or address noted on the form. Web when submitting a provider reconsideration or administrative appeal, please complete the form in its entirety in accordance with the instructions contained in.
TN BCBS 19PED504697 20192021 Fill and Sign Printable Template Online
Web when submitting a provider reconsideration or administrative appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for physician and providers available online at floridablue.com. Web please submit reconsideration requests in writing. Original claims should not be attached to a review form. Manufacturers invoice for pricing (attached)copy of subrogation or worker's.
Bcbs Reconsideration Form Texas
Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Web provider reconsideration helpful guide; Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request. Web please submit reconsideration requests.
270 Bcbs Forms And Templates free to download in PDF
Specialty pharmacy / advanced therapeutics authorizations; Reason for reconsideration (mark applicable box): Do not use this form to submit a corrected claim or to respond to an additional information request from. Most provider appeal requests are related to a length of stay or treatment setting denial. Here are other important details you need to know about this form:
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
Web please submit reconsideration requests in writing. Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request. Do not use this form to submit a corrected claim or to respond to an additional information request from. Web this form is only.
Bcbs Prior Authorization Form Medication Form Resume Examples
Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Access and download these helpful bcbstx health care provider forms. A request to blue cross and blue shield of nebraska (bcbsne) to review a claim with additional information not previously provided. Only one reconsideration is allowed per claim. Web.
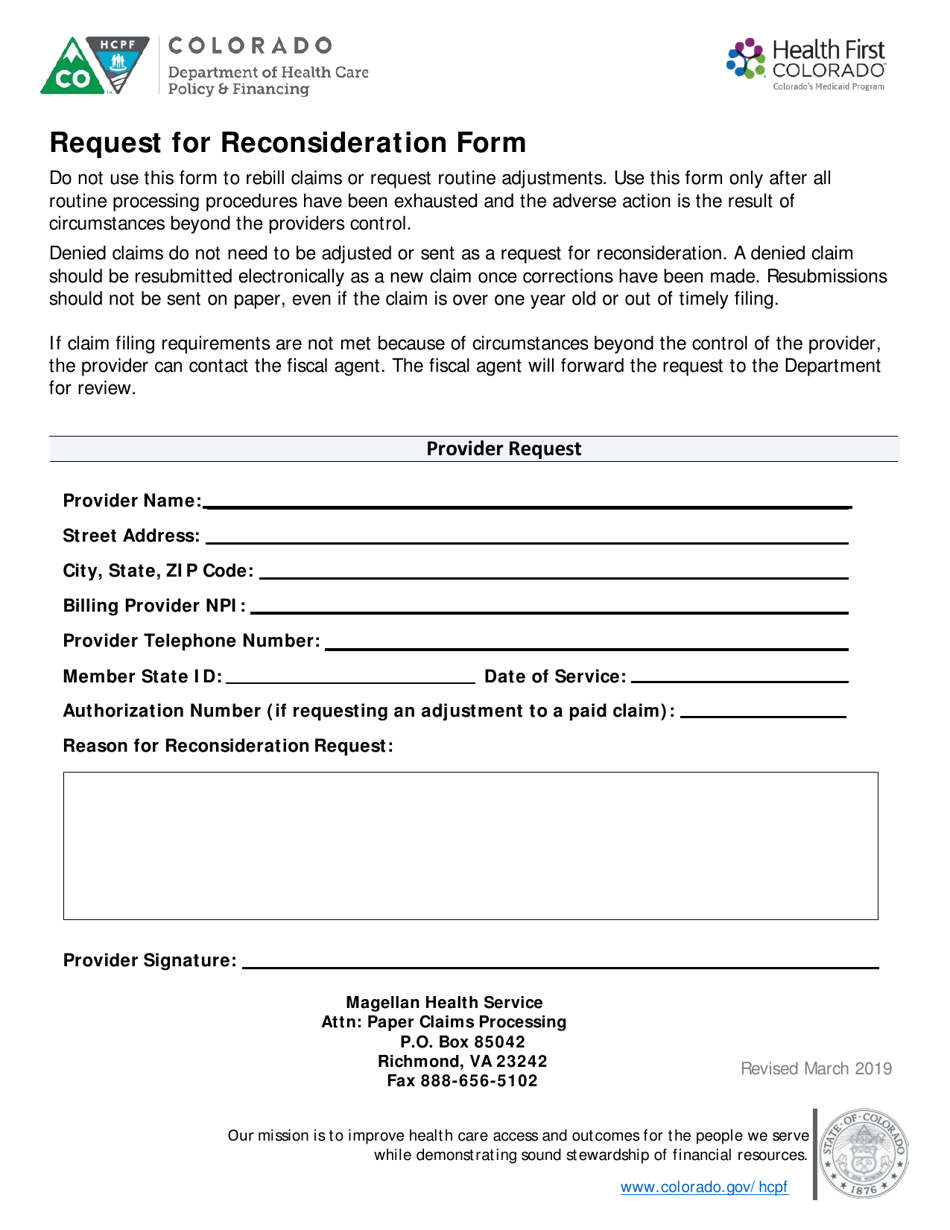
Colorado Request for Reconsideration Form Download Printable PDF
For additional information and requirements regarding provider Do not use this form to submit a corrected claim or to respond to an additional information request from. Specialty pharmacy / advanced therapeutics authorizations; Original claims should not be attached to a review form. Only one reconsideration is allowed per claim.
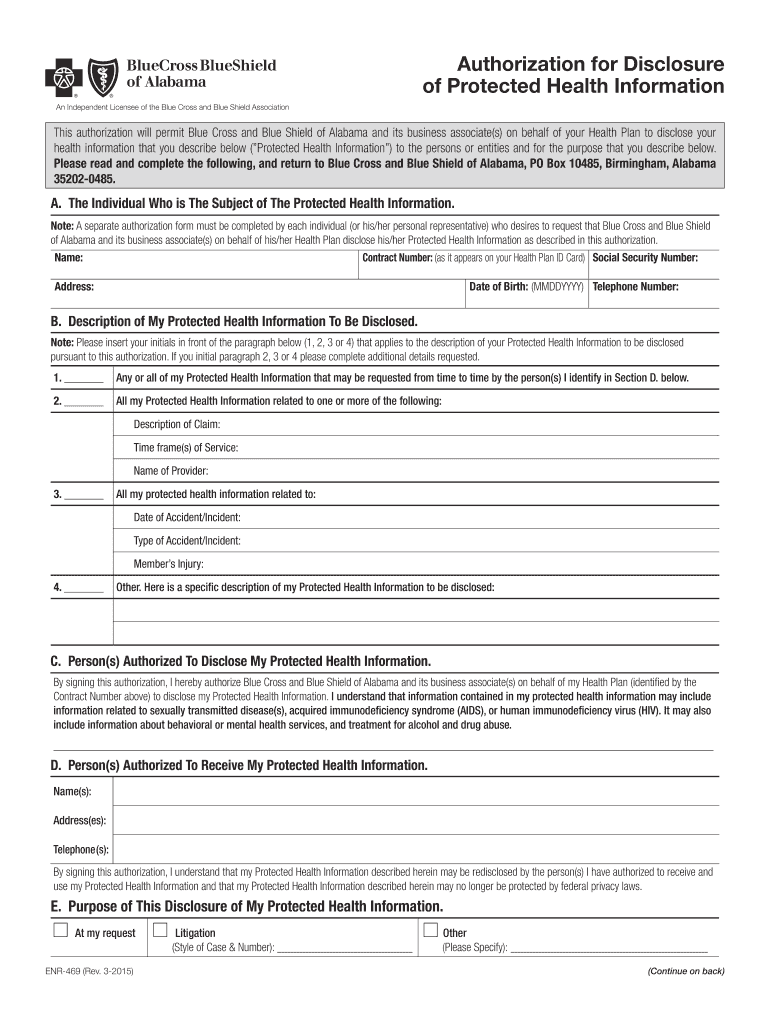
AL BCBS Form ENR469 20152021 Fill and Sign Printable Template
Manufacturers invoice for pricing (attached)copy of subrogation or worker's compensation* Only one reconsideration is allowed per claim. Access and download these helpful bcbstx health care provider forms. Send the form and supporting materials to the appropriate fax number or address noted on the form. Web provider reconsideration form please use this form if you have questions or disagree about a.
Specialty Pharmacy / Advanced Therapeutics Authorizations;
Web please submit reconsideration requests in writing. A request to blue cross and blue shield of nebraska (bcbsne) to review a claim with additional information not previously provided. Web provider reconsideration helpful guide; Skilled nursing facility rehab form ;
Original Claims Should Not Be Attached To A Review Form.
Web this form is for all providers requesting information about claims status or disputing a claim with blue cross and blue shield of illinois (bcbsil) and serving members in the state of illinois. Send the form and supporting materials to the appropriate fax number or address noted on the form. Radiation oncology therapy cpt codes; Manufacturers invoice for pricing (attached)copy of subrogation or worker's compensation*
Web Blue Cross Blue Shield Of Texas Is Committed To Giving Health Care Providers With The Support And Assistance They Need.
Most provider appeal requests are related to a length of stay or treatment setting denial. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Here are other important details you need to know about this form: Web provider reconsideration form please use this form if you have questions or disagree about a payment, and attach it to any supporting documentation related to your reconsideration request.
Reason For Reconsideration (Mark Applicable Box):
Do not use this form to submit a corrected claim or to respond to an additional information request from. This is different from the request for claim review request process outlined above. Web when submitting a provider reconsideration or administrative appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for physician and providers available online at floridablue.com. Web this form is only to be used for review of a previously adjudicated claim.