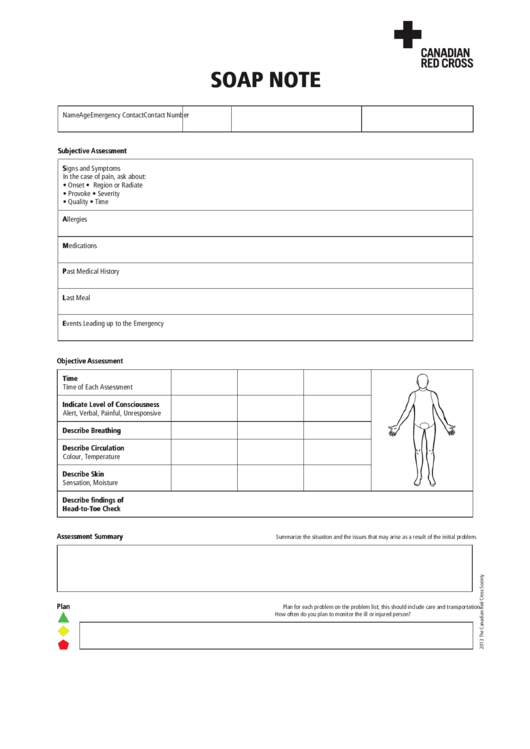
Soap Note Template Pdf
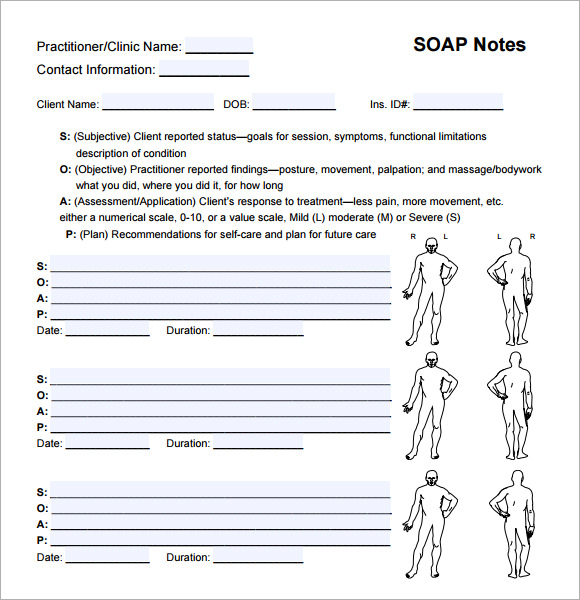
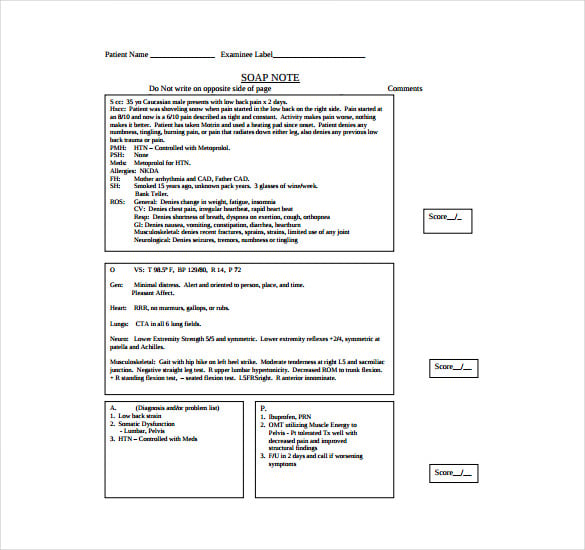
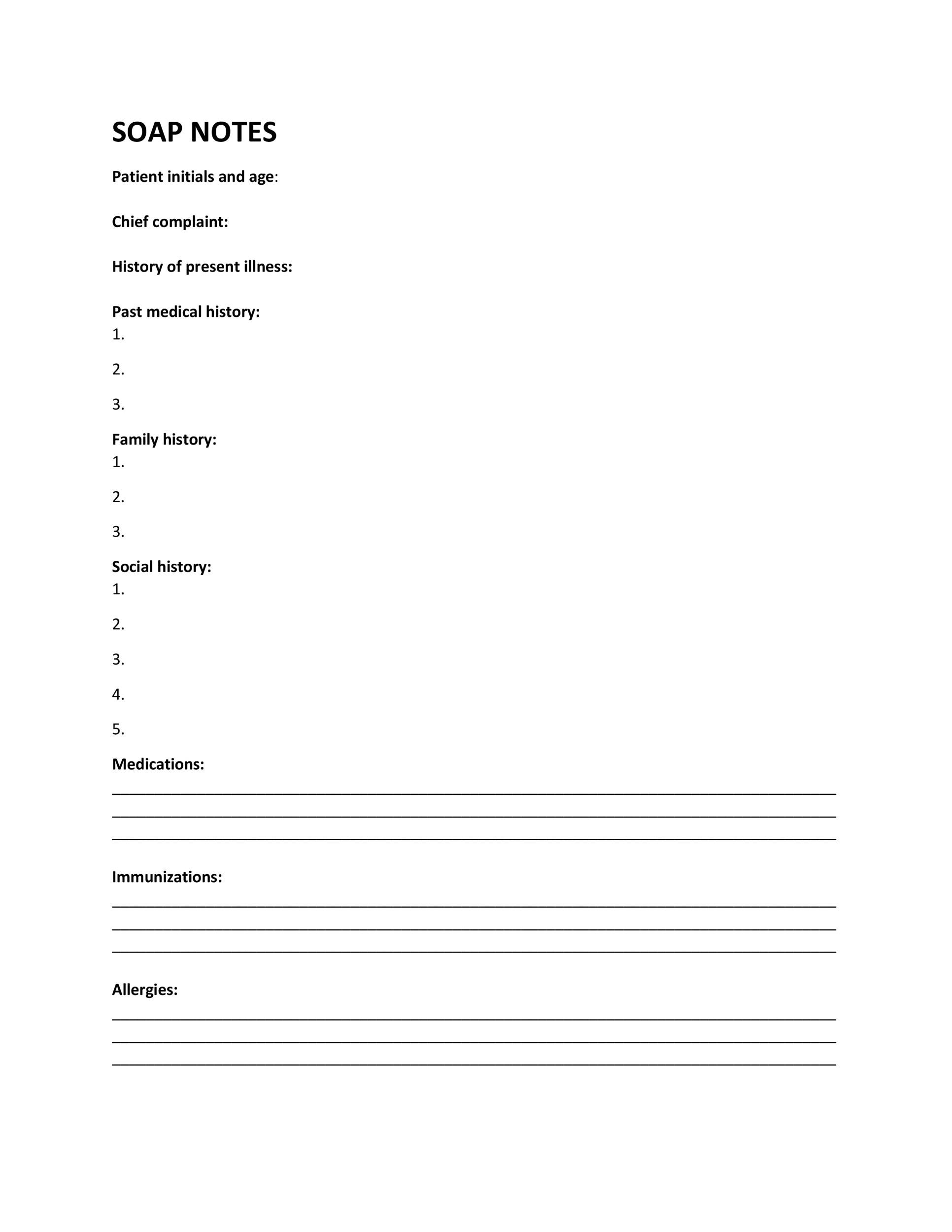
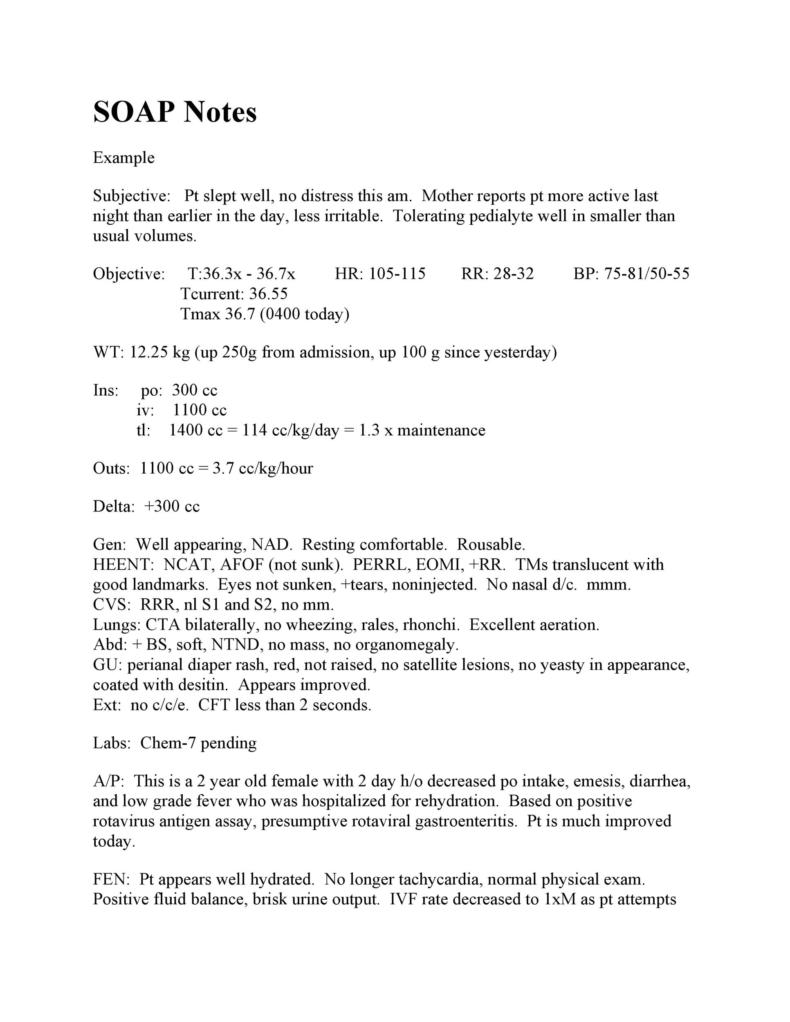
Soap Note Template Pdf - Good turgor, no rash, unusual bruising or prominent lesions hair: Web clinical soap note format the “history” section hpi: (listed are the components of the all normal physical exam) general: Web start using template. Web 3 helpful templates and formats with a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your p rogress notes, as well as the speed with which you write them. Use this template for creating concise patient documentation to develop accurate solutions. This website offers free soap notes templates for pediatrics and nursing. Web one of the most common and effective techniques to document a session is called writing soap notes. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more.
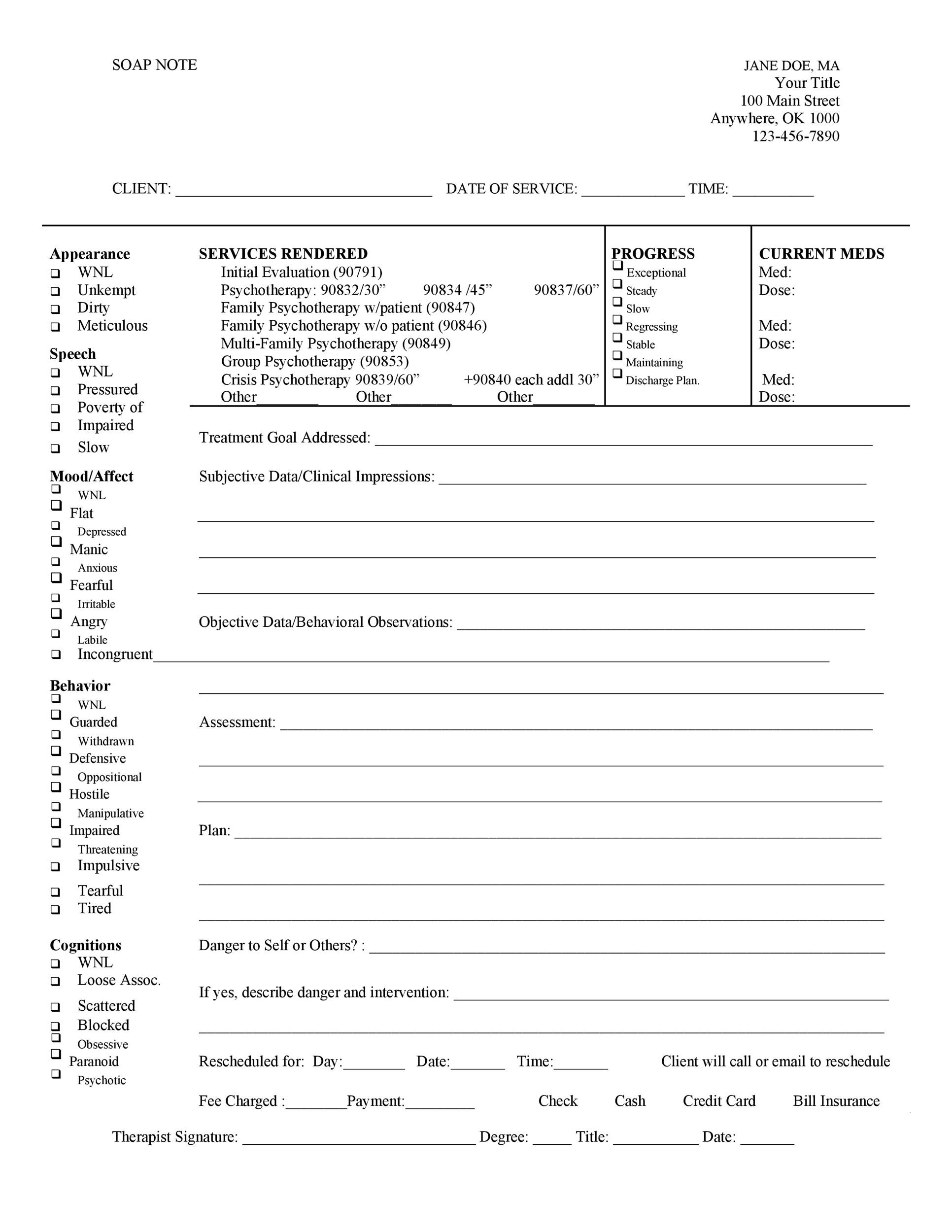
Web the soap note format helps medical professionals to record patient data easily through a highly structured style. Here’s how to write soap notes. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Web start using template. In this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Web one of the most common and effective techniques to document a session is called writing soap notes. Client was tearful during session with a sad affect and required pauses in. This soap note template is a documentation format used by physicians and other health care professionals to assess patient conditions. Web clinical soap note format the “history” section hpi:
Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Follow the points below to utilize this template: Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). This soap note template is a documentation format used by physicians and other health care professionals to assess patient conditions. Web one of the most common and effective techniques to document a session is called writing soap notes. Web \\cluster1\home\nancy.clark\1 training\emr\soap note.doc o: This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more. Well appearing, well nourished, in no distress.oriented x 3, normal mood and affect. Client was tearful during session with a sad affect and required pauses in. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient).
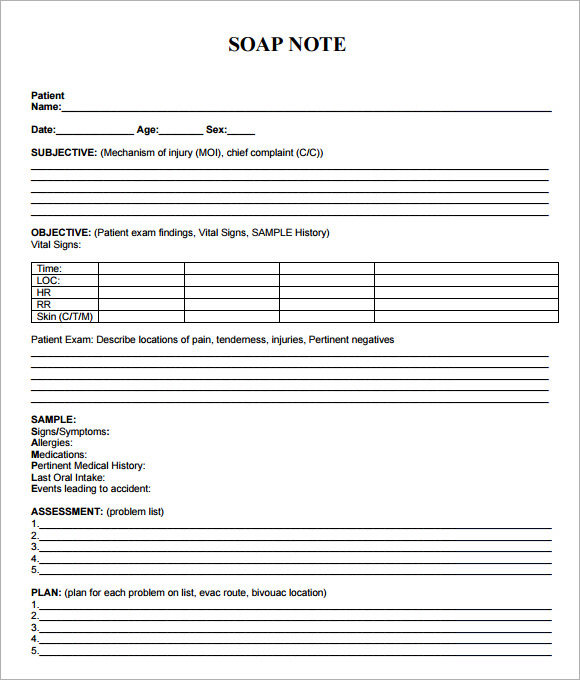
10+ Soap Note Template Free Download Word, Excel, PDF Format!!
Web clinical soap note format the “history” section hpi: This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information (listed are the components of the all normal physical exam) general: Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Well appearing,.
FREE 8+ Sample Soap Note Templates in MS Word PDF
Here’s how to write soap notes. Well appearing, well nourished, in no distress.oriented x 3, normal mood and affect. Web one of the most common and effective techniques to document a session is called writing soap notes. Web the soap note format helps medical professionals to record patient data easily through a highly structured style. Web clinical soap note format.
Soap Note Template 9+ Free Word, PDF Format Download! Free
Good turgor, no rash, unusual bruising or prominent lesions hair: This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always.
40 Fantastic SOAP Note Examples & Templates Template Lab
Here’s how to write soap notes. This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information Follow the points below to utilize this template: Web one of the most common and effective techniques to document a session is called writing soap notes. Web start using template.
Soap Note Template Pdf Luxury soap Note Template 9 Free Word Pdf format
Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Web start using template. Use this template for creating concise patient documentation to develop accurate solutions. Web \\cluster1\home\nancy.clark\1 training\emr\soap note.doc o: This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
Download our comprehensive soap note pdf template for mental health professionals and other. Well appearing, well nourished, in no distress.oriented x 3, normal mood and affect. Web clinical soap note format the “history” section hpi: Good turgor, no rash, unusual bruising or prominent lesions hair: Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify.
Soap Note Template printable pdf download
Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). In this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Web start using template. Well appearing, well nourished, in.
FREE 8+ Sample Soap Note Templates in MS Word PDF
Download our comprehensive soap note pdf template for mental health professionals and other. (listed are the components of the all normal physical exam) general: This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more. Here’s how to write soap notes. Web \\cluster1\home\nancy.clark\1 training\emr\soap note.doc o:
Icu Soap Note Template PDF Template
This website offers free soap notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more. Here’s how to write soap notes. Web 3 helpful templates and formats with a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your p rogress notes, as well as the speed with which you.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
Download our comprehensive soap note pdf template for mental health professionals and other. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). (listed are the components of the all normal physical exam) general: Web start using template. The formats for downloading the templates are doc and pdf and the.
Follow The Points Below To Utilize This Template:
This soap note template is a documentation format used by physicians and other health care professionals to assess patient conditions. Download our comprehensive soap note pdf template for mental health professionals and other. Web the soap note format helps medical professionals to record patient data easily through a highly structured style. (listed are the components of the all normal physical exam) general:
Include Symptom Dimensions, Chronological Narrative Of Patient’s Complains, Information Obtained From Other Sources (Always Identify Source If Not The Patient).
The formats for downloading the templates are doc and pdf and the file size starts from 8kb. Web \\cluster1\home\nancy.clark\1 training\emr\soap note.doc o: This website offers free soap notes templates for pediatrics and nursing. Use this template for creating concise patient documentation to develop accurate solutions.
In This Post, We Will Review What Soap Notes Are, How To Write A Soap Note, Tips For Effective Soap Notes, And A Template You Can Use For Your Soap Notes.
This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information Web 3 helpful templates and formats with a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your p rogress notes, as well as the speed with which you write them. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Web start using template.
Web One Of The Most Common And Effective Techniques To Document A Session Is Called Writing Soap Notes.
Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Here’s how to write soap notes. Good turgor, no rash, unusual bruising or prominent lesions hair: Well appearing, well nourished, in no distress.oriented x 3, normal mood and affect.