Optumrx Tier Exception Form
Optumrx Tier Exception Form - Web prescription drug prior authorization or step therapy exception request form patient name: Generic medications are shown in lowercase (for example, clobetasol). Optumrx is not authorized to review requests for medications supplied by the physician’s office. Web fill out every fillable field. Forms are updated frequently and may be barcoded. Web this form may be sent to us by mail or fax: Who may make a request: Do not copy for future use. Use the cross or check marks in the top toolbar to select your answers in the list boxes. Web partial copay waiver (pcw) exception prior authorization request form.
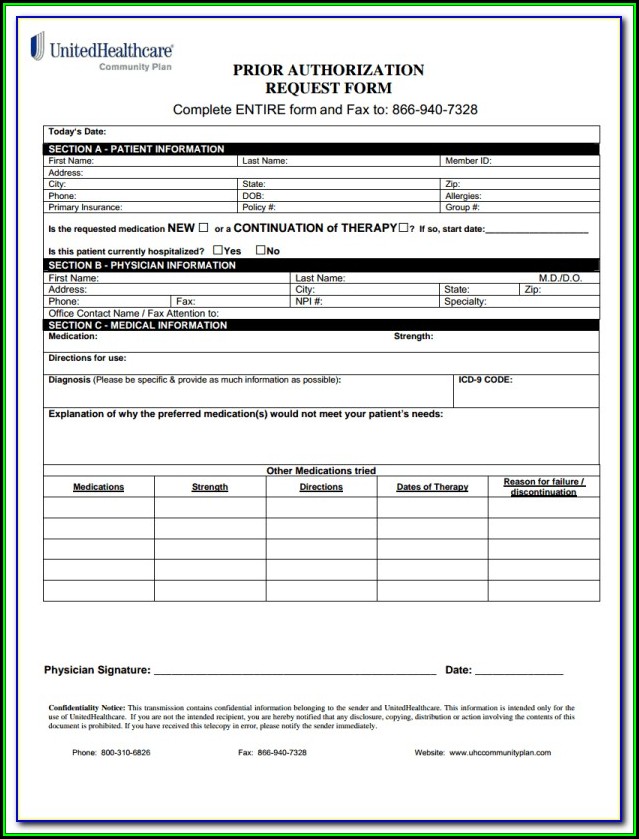
Web to submit a tiering exception, copay waiver, tier cost sharing, or any other cost reductions requests (e.g., hcr), please contact the optumrx® pa department through telephone or fax. Click on the sign tool and make a signature. Include the date to the form using the date feature. Start completing the fillable fields and carefully type in required information. Who may make a request: Use get form or simply click on the template preview to open it in the editor. You may also ask us for a coverage determination by calling the member services number on the back of your id card. Forms are updated frequently and may be barcoded Forms are updated frequently and may be barcoded. You can ask the plan to cover your drug even if it is not on the plan's drug list (formulary).
Click on the sign tool and make a signature. Include the date to the form using the date feature. Start completing the fillable fields and carefully type in required information. Web optumrx tier exception form is a request form that allows a patient to request a medication that is a higher tier on their insurance formulary. Who may make a request: Web partial copay waiver (pcw) exception prior authorization request form. Use the cross or check marks in the top toolbar to select your answers in the list boxes. Web to submit a tiering exception, copay waiver, tier cost sharing, or any other cost reductions requests (e.g., hcr), please contact the optumrx® pa department through telephone or fax. Please fill out all applicable sections on both pages completely and legibly. Web fill out every fillable field.
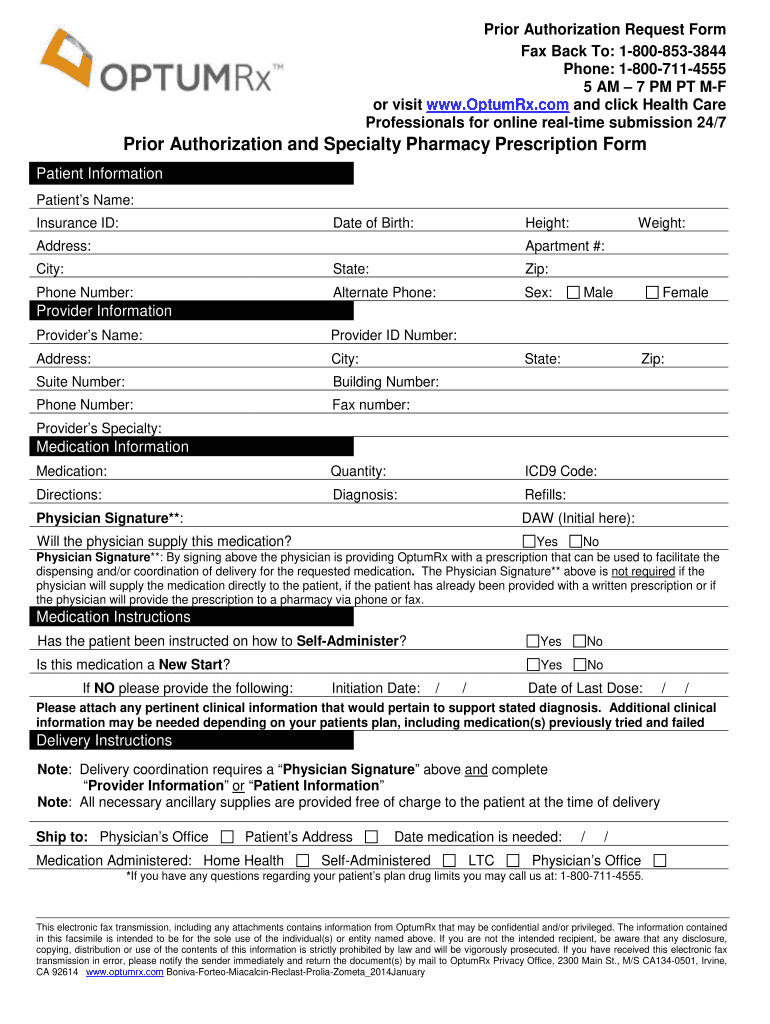
Optum Rx Pa Form Fill Out and Sign Printable PDF Template signNow
Web optumrx tier exception form is a request form that allows a patient to request a medication that is a higher tier on their insurance formulary. Forms are updated frequently and may be barcoded. Click on the sign tool and make a signature. You may also ask us for a coverage determination by calling the member services number on the.
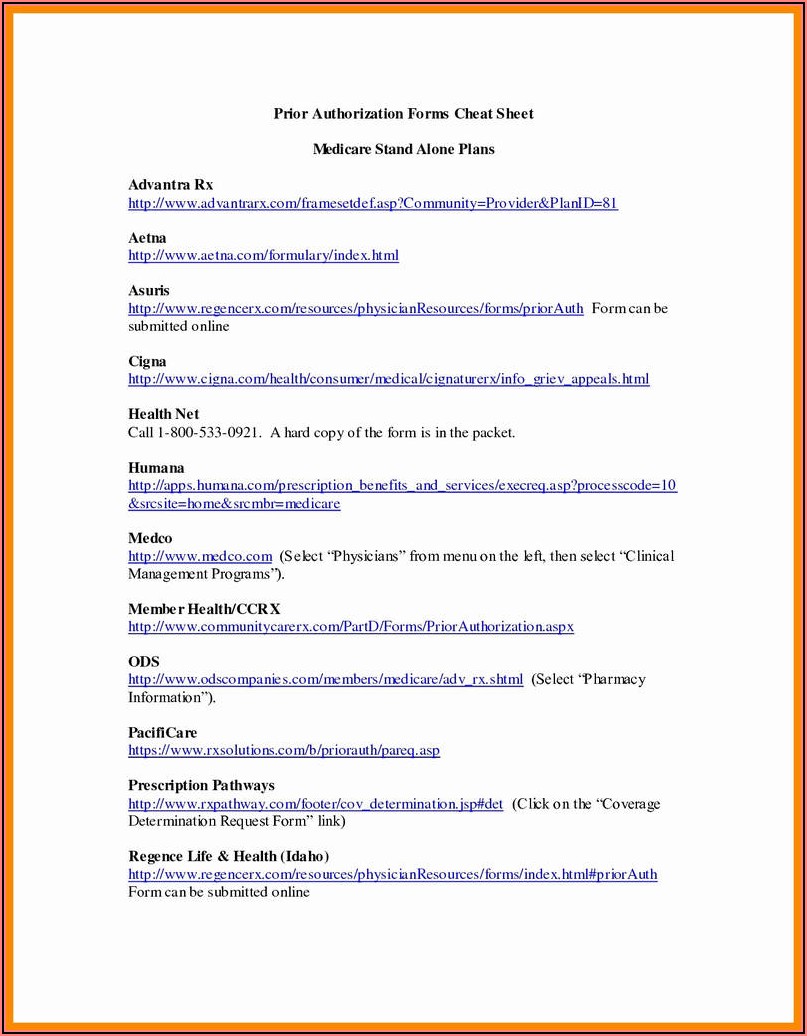
Optumrx Medicare Part D Tier Exception Form Form Resume Examples
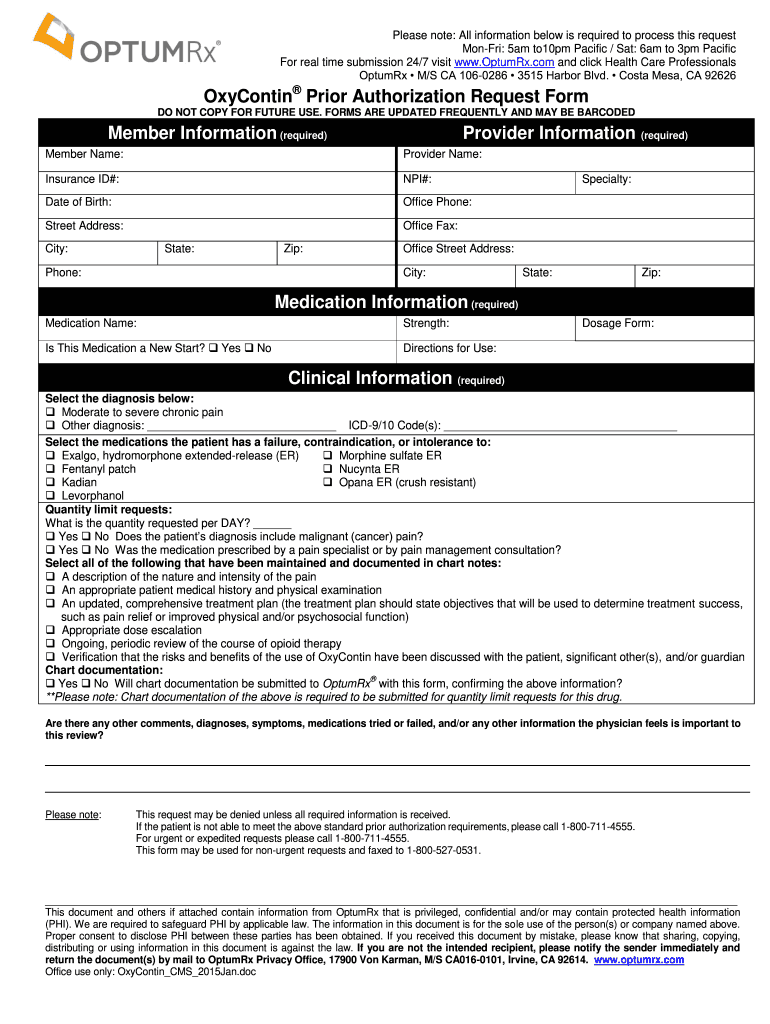
Optumrx is not authorized to review requests for medications supplied by the physician’s office. Web optumrx tier exception form is a request form that allows a patient to request a medication that is a higher tier on their insurance formulary. Member information (required) provider information (required) member name: Web prescription drug prior authorization or step therapy exception request form patient.
Optumrx Prior Authorization Form Cialis — Pharmacy General Exception Forms
Optumrx is not authorized to review requests for medications supplied by the physician’s office. Use get form or simply click on the template preview to open it in the editor. Web prescription drug prior authorization or step therapy exception request form patient name: Web fill out every fillable field. Please fill out all applicable sections on both pages completely and.
Optumrx Medicare Part D Tier Exception Form Form Resume Examples
Start completing the fillable fields and carefully type in required information. Include the date to the form using the date feature. Web partial copay waiver (pcw) exception prior authorization request form. Use get form or simply click on the template preview to open it in the editor. Forms are updated frequently and may be barcoded.
Optumrx Prior Authorization Form Cialis Rx Prior Authorization
Click on the sign tool and make a signature. Forms are updated frequently and may be barcoded Web prescription drug prior authorization or step therapy exception request form patient name: Web partial copay waiver (pcw) exception prior authorization request form. Include the date to the form using the date feature.
2014 OPTUMRx Nuvigil & Provigil Prior Authorization Request Form Fill
Forms are updated frequently and may be barcoded. Who may make a request: You can't ask for an exception to the copayment or coinsurance amount you're required to pay for the drug. Web partial copay waiver (pcw) exception prior authorization request form. Include the date to the form using the date feature.
Optumrx Medicare Part D Electronic Prior Authorization form Brilliant
Do not copy for future use. You can't ask for an exception to the copayment or coinsurance amount you're required to pay for the drug. Member information (required) provider information (required) member name: Web to submit a tiering exception, copay waiver, tier cost sharing, or any other cost reductions requests (e.g., hcr), please contact the optumrx® pa department through telephone.
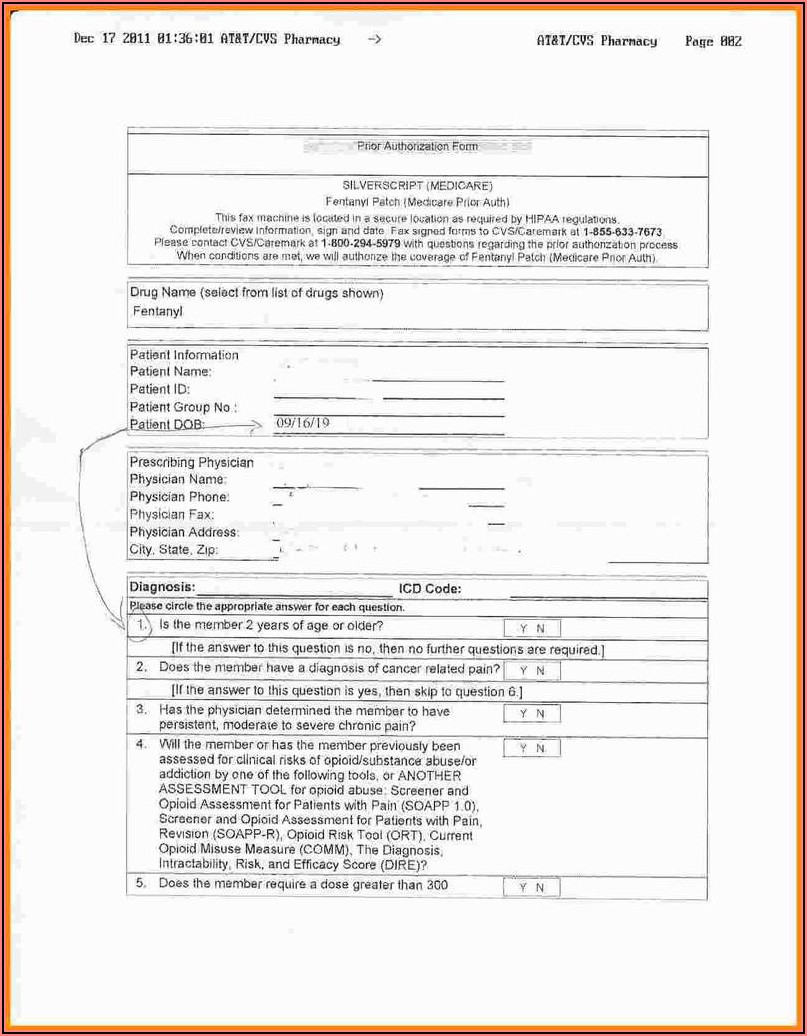
Optum rx oxycontin pa form Fill Out and Sign Printable PDF Template
Use the cross or check marks in the top toolbar to select your answers in the list boxes. Click on the sign tool and make a signature. Include the date to the form using the date feature. Web to submit a tiering exception, copay waiver, tier cost sharing, or any other cost reductions requests (e.g., hcr), please contact the optumrx®.
Cvs Caremark Tier Exception Form
Web this form may be sent to us by mail or fax: Web optumrx tier exception form is a request form that allows a patient to request a medication that is a higher tier on their insurance formulary. You can ask the plan to cover your drug even if it is not on the plan's drug list (formulary). Generic medications.
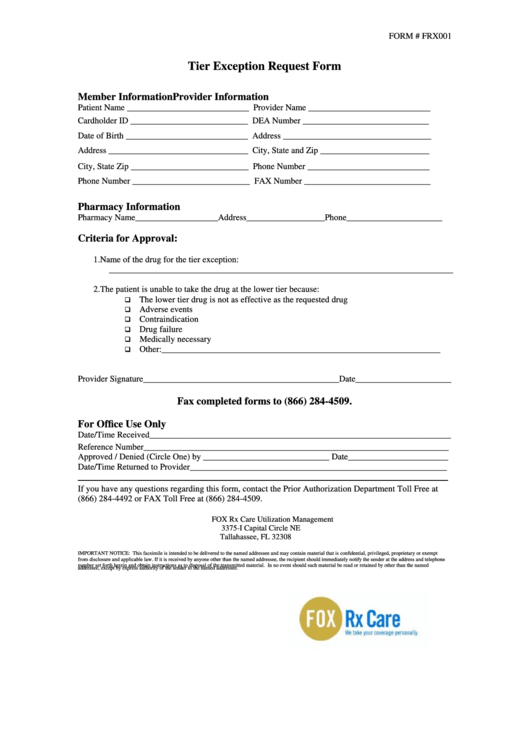
Form Frx001 Tier Exception Request Form printable pdf download
Please fill out all applicable sections on both pages completely and legibly. Use the cross or check marks in the top toolbar to select your answers in the list boxes. Web fill out every fillable field. You can't ask for an exception to the copayment or coinsurance amount you're required to pay for the drug. Forms are updated frequently and.
Use The Cross Or Check Marks In The Top Toolbar To Select Your Answers In The List Boxes.
Web optumrx tier exception form is a request form that allows a patient to request a medication that is a higher tier on their insurance formulary. Web to submit a tiering exception, copay waiver, tier cost sharing, or any other cost reductions requests (e.g., hcr), please contact the optumrx® pa department through telephone or fax. Web partial copay waiver (pcw) exception prior authorization request form. Generic medications are shown in lowercase (for example, clobetasol).
Web This Form May Be Sent To Us By Mail Or Fax:
Your plan may have multiple or no tiers. Optumrx is not authorized to review requests for medications supplied by the physician’s office. Please fill out all applicable sections on both pages completely and legibly. You may also ask us for a coverage determination by calling the member services number on the back of your id card.
Forms Are Updated Frequently And May Be Barcoded
Who may make a request: You can't ask for an exception to the copayment or coinsurance amount you're required to pay for the drug. Use get form or simply click on the template preview to open it in the editor. Include the date to the form using the date feature.
Click On The Sign Tool And Make A Signature.
Do not copy for future use. You can ask the plan to cover your drug even if it is not on the plan's drug list (formulary). Forms are updated frequently and may be barcoded. Member information (required) provider information (required) member name: