Cigna Provider Appeal Form
Cigna Provider Appeal Form - Payment issue duplicate claim retraction of payment request for medical records • include copy of letter/request received Web quickly locate the forms you need for authorizations, referrals, or filing or appealing claims with our forms resource area. Complete and mail this form and/or appeal letter along with all supporting documentation to the address identified in step 3 on this form. Fields with an asterisk ( * ) are required. Your appeal should be submitted within 180 days and allow 60 days for processing your appeal, unless other timelines are required by state law. Be specific when completing the description of dispute and expected outcome. Resulted in the claim not being paid at all for reasons other than a um determination or a determination of ineligibility, coordination of benefits or fraud investigation Following is a checklist of information required: Web how to submit an appeal fill out the request for health care provider payment review form [pdf]. Complete claim make sure the claim form includes all critical information needed for cigna to process.
Web quickly locate the forms you need for authorizations, referrals, or filing or appealing claims with our forms resource area. The form will help to fully document the circumstances around the appeal request and will also help to ensure a timely review of the appeal. Web instructions please complete the below form. Web how to submit an appeal fill out the request for health care provider payment review form [pdf]. Payment issue duplicate claim retraction of payment request for medical records • include copy of letter/request received Provide additional information to support the description of the dispute. Web cigna strives to informally resolve issues raised by health care providers on initial contact whenever possible. Following is a checklist of information required: We may be able to resolve your issue quickly outside of the formal appeal process. Your appeal should be submitted within 180 days and allow 60 days for processing your appeal, unless other timelines are required by state law.
Provide additional information to support the description of the dispute. The form will help to fully document the circumstances around the appeal request and will also help to ensure a timely review of the appeal. Complete and mail this form and/or appeal letter along with all supporting documentation to the address identified in step 3 on this form. Login.quickaccesslink.resources.coveragetitle access information on cigna standard health coverage plan provisions and medical coverage policies with our extensive coverage policies resource area. Web instructions please complete the below form. If issues cannot be resolved informally, cigna offers two options: Be specific when completing the description of dispute and expected outcome. Your appeal should be submitted within 180 days and allow 60 days for processing your appeal, unless other timelines are required by state law. Do not include a copy of a claim that was previously processed. Resulted in the claim not being paid at all for reasons other than a um determination or a determination of ineligibility, coordination of benefits or fraud investigation
Cigna Logo PNG Image PurePNG Free transparent CC0 PNG Image Library
Login.quickaccesslink.resources.coveragetitle access information on cigna standard health coverage plan provisions and medical coverage policies with our extensive coverage policies resource area. Under america's healthcare system, such as it is, a medical patient typically sees a doctor and receives diagnosis and possibly treatment. Provide additional information to support the description of the dispute. Complete and mail this form and/or appeal letter.
Cigna Evidence Of Insurability Form Sanepo
Under america's healthcare system, such as it is, a medical patient typically sees a doctor and receives diagnosis and possibly treatment. Web quickly locate the forms you need for authorizations, referrals, or filing or appealing claims with our forms resource area. Web instructions please complete the below form. Fields with an asterisk ( * ) are required. Appeals unit po.
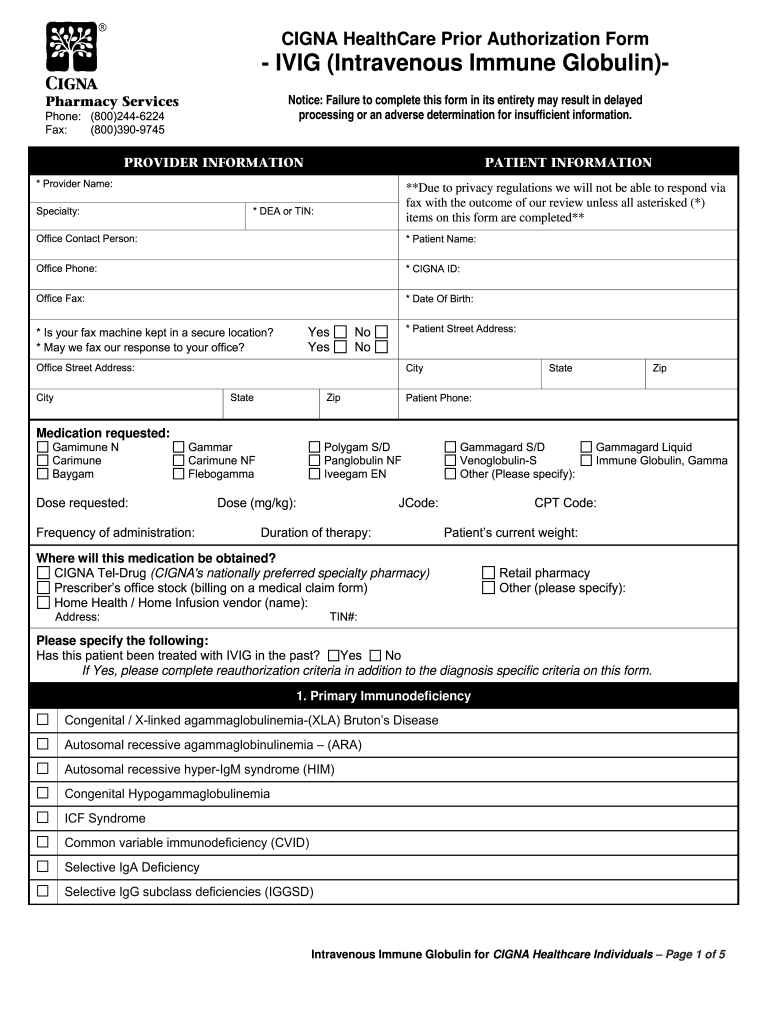
Cigna Ivig Auth Fill Out and Sign Printable PDF Template signNow
Your appeal should be submitted within 180 days and allow 60 days for processing your appeal, unless other timelines are required by state law. Be specific when completing the description of dispute and expected outcome. Web cigna strives to informally resolve issues raised by health care providers on initial contact whenever possible. Requests for review should include: Under america's healthcare.
Health Plan of San Mateo Prior Authorization Form Fill Out and Sign
Do not include a copy of a claim that was previously processed. Login.quickaccesslink.resources.coveragetitle access information on cigna standard health coverage plan provisions and medical coverage policies with our extensive coverage policies resource area. Appeals unit po box 24087 nashville, tn 37202 fax: Under america's healthcare system, such as it is, a medical patient typically sees a doctor and receives diagnosis.
360 View of Cigna Healthspring Strategies for Improving Provider
Appeals unit po box 24087 nashville, tn 37202 fax: Web how to submit an appeal fill out the request for health care provider payment review form [pdf]. Be specific when completing the description of dispute and expected outcome. Provide additional information to support the description of the dispute. Payment issue duplicate claim retraction of payment request for medical records •.
Cigna Insurance Appeal Fill Online, Printable, Fillable, Blank
Requests for review should include: Web instructions please complete the below form. The form will help to fully document the circumstances around the appeal request and will also help to ensure a timely review of the appeal. Following is a checklist of information required: Cigna has been sued in california based on allegations the us healthcare insurer unlawfully reviewed insurance.
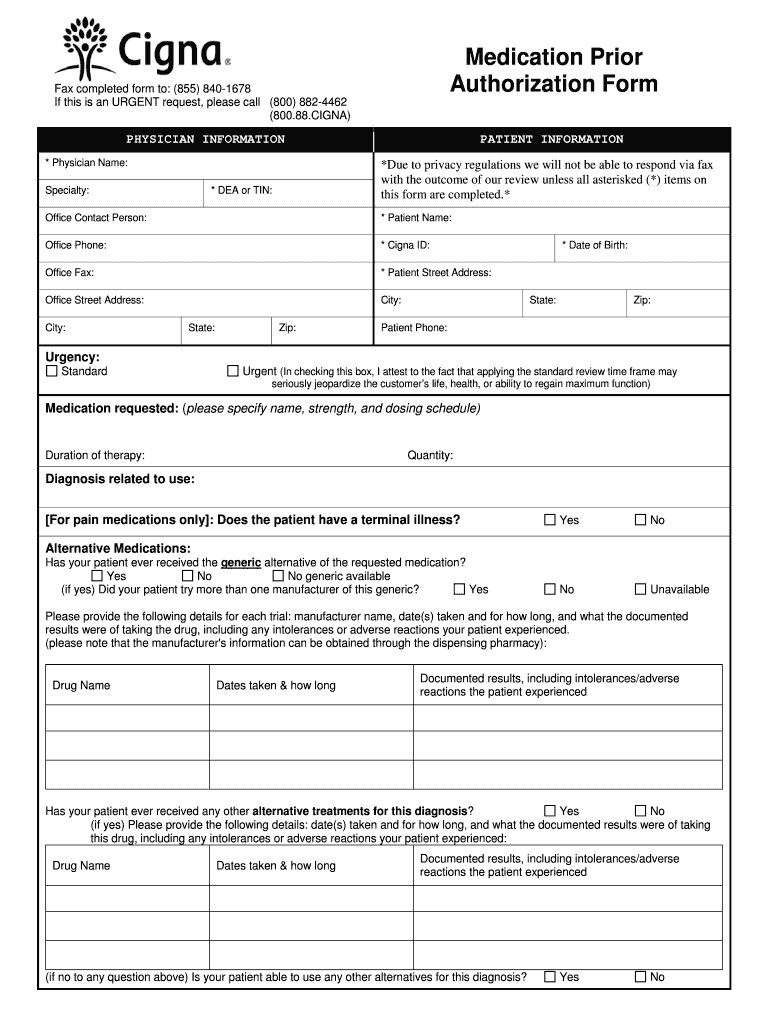
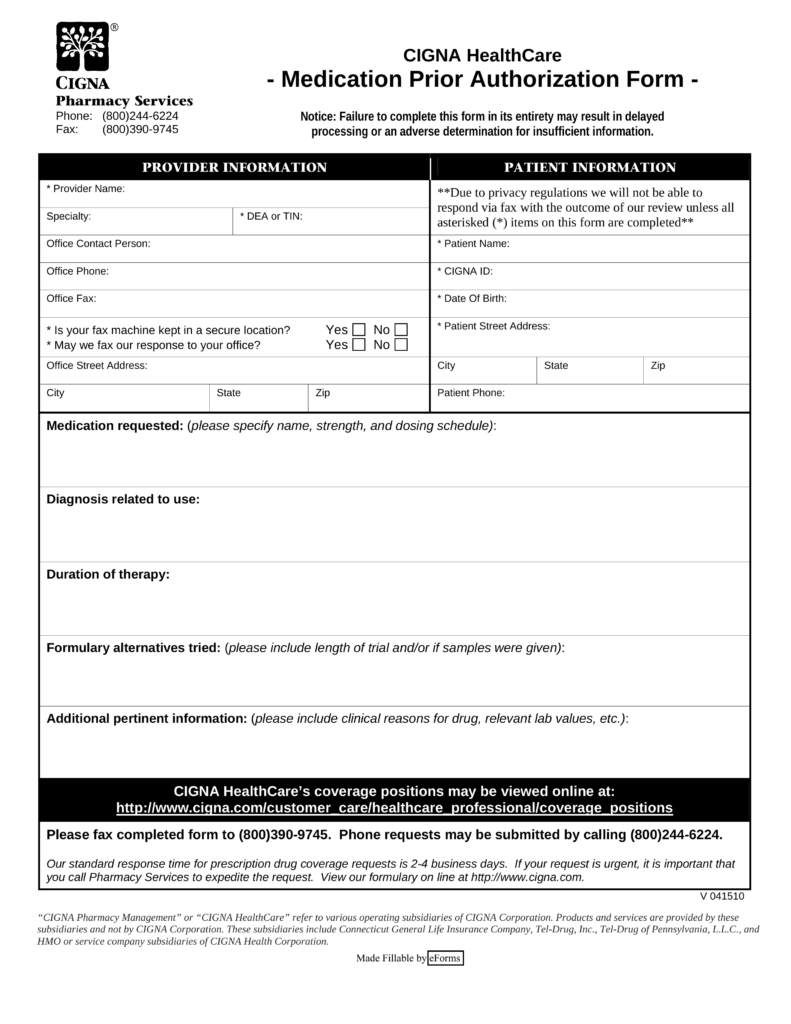
Free Cigna Prior (Rx) Authorization Form PDF eForms
Be specific when completing the description of dispute and expected outcome. Login.quickaccesslink.resources.coveragetitle access information on cigna standard health coverage plan provisions and medical coverage policies with our extensive coverage policies resource area. Web quickly locate the forms you need for authorizations, referrals, or filing or appealing claims with our forms resource area. Resulted in the claim not being paid at.
Fill Free fillable Cigna Medicare Providers PDF forms
Web cigna strives to informally resolve issues raised by health care providers on initial contact whenever possible. Complete claim make sure the claim form includes all critical information needed for cigna to process. We may be able to resolve your issue quickly outside of the formal appeal process. Provide additional information to support the description of the dispute. Under america's.
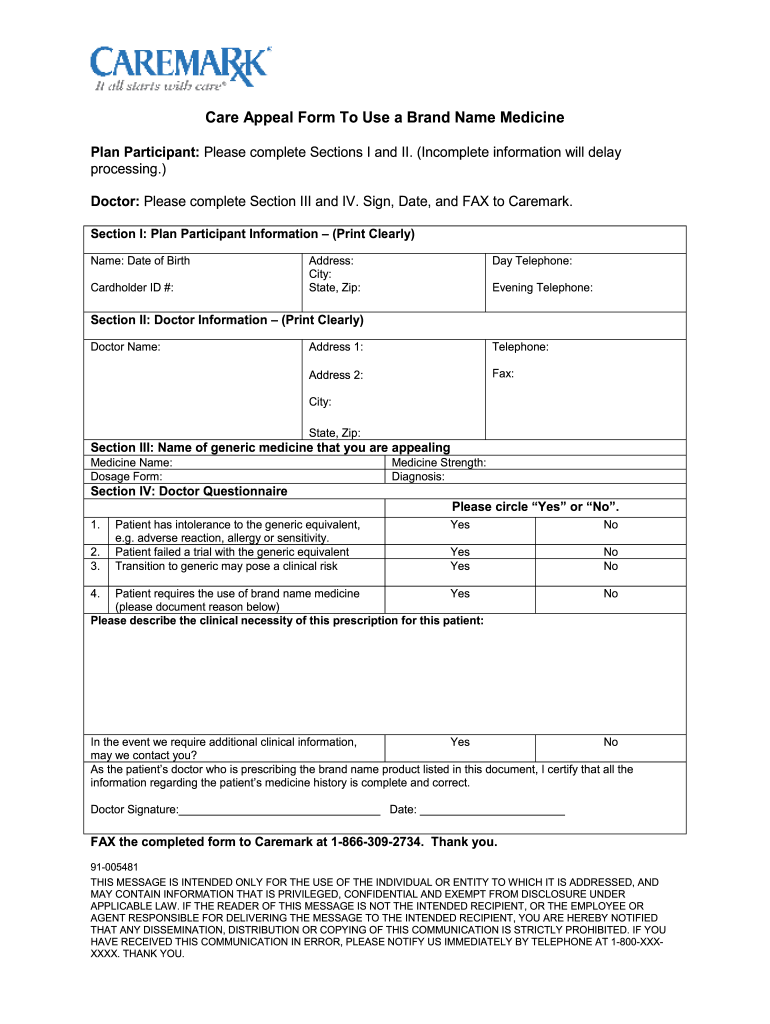
What Is My Cvs Caremark Id Number medicamentomelatonininfo
Web wed 26 jul 2023 // 21:13 utc. Be specific when completing the description of dispute and expected outcome. We may be able to resolve your issue quickly outside of the formal appeal process. Fields with an asterisk ( * ) are required. Web you may submit a health care professional application to appeal a claims determination if our determination:
Cigna Healthspring 50 Gift Card Form Fill Online, Printable, Fillable
Web instructions please complete the below form. Web cigna strives to informally resolve issues raised by health care providers on initial contact whenever possible. We may be able to resolve your issue quickly outside of the formal appeal process. Web you may submit a health care professional application to appeal a claims determination if our determination: Cigna has been sued.
Web Wed 26 Jul 2023 // 21:13 Utc.
Do not include a copy of a claim that was previously processed. Requests for review should include: Web how to submit an appeal fill out the request for health care provider payment review form [pdf]. Login.quickaccesslink.resources.coveragetitle access information on cigna standard health coverage plan provisions and medical coverage policies with our extensive coverage policies resource area.
Your Appeal Should Be Submitted Within 180 Days And Allow 60 Days For Processing Your Appeal, Unless Other Timelines Are Required By State Law.
Web you may submit a health care professional application to appeal a claims determination if our determination: Web cigna strives to informally resolve issues raised by health care providers on initial contact whenever possible. We may be able to resolve your issue quickly outside of the formal appeal process. Be specific when completing the description of dispute and expected outcome.
Payment Issue Duplicate Claim Retraction Of Payment Request For Medical Records • Include Copy Of Letter/Request Received
Resulted in the claim not being paid at all for reasons other than a um determination or a determination of ineligibility, coordination of benefits or fraud investigation Web instructions please complete the below form. If issues cannot be resolved informally, cigna offers two options: Appeals unit po box 24087 nashville, tn 37202 fax:
Under America's Healthcare System, Such As It Is, A Medical Patient Typically Sees A Doctor And Receives Diagnosis And Possibly Treatment.
Fields with an asterisk ( * ) are required. Complete claim make sure the claim form includes all critical information needed for cigna to process. Cigna has been sued in california based on allegations the us healthcare insurer unlawfully reviewed insurance claims using automated systems rather than relying on humans. Provide additional information to support the description of the dispute.